This article originally appeared in Clinical Practice Today.
Polycystic ovary syndrome (PCOS), a chronic condition lasting from adolescence to menopause, often goes unrecognized, and its diagnosis is sometimes difficult. Although the majority of women presenting with the syndrome’s hallmark symptoms of irregular menses and hyperandrogenism will have PCOS, Duke endocrinologists are encouraging physicians to examine symptoms more closely to ensure there is no evidence of other, less common causes.
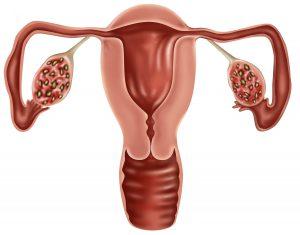
PCOS is now recognized as the most common endocrine disorder among women of reproductive age, affecting 6% to 15% of this population, depending on the diagnostic criteria used. Although guidelines differ, a diagnosis of PCOS requires a combination of at least 2 of the following 3 elements: ovulatory dysfunction, hyperandrogenism (clinical or biochemical), and ovarian morphology (confirmation on pelvic ultrasonography).
“Up to 20% of all women will present with classic PCOS appearance on pelvic ultrasound, yet they have normal ovulatory cycles and no hyperandrogenism,” says endocrine nurse practitioner Katherine Pereira, DNP. “While there are specific criteria as to what an ultrasound must find and measure, it cannot be used as the sole measure for confirming a diagnosis. Further investigation is warranted before confirming a diagnosis and, when the diagnosis is not clear, the patient should be referred to an endocrinologist.”
Ann Brown, MD, MHS, an endocrinologist who also holds an appointment in obstetrics and gynecology, agrees: “We go through a checklist and break down our patients’ symptoms. For a diagnosis of PCOS, there have to be signs of irregular ovulation and some element of excess androgen. But how do you determine the cause of these symptoms? Should you also be thinking of other unusual causes for these symptoms?”
A pituitary tumor, for example, may cause amenorrhea, while high prolactin levels might indicate prolactinoma. Elevated androgen levels could be caused by an androgen-secreting tumor, and increased cortisol levels might indicate Cushing syndrome. Other causes of PCOS-like symptoms might include late-onset congenital adrenal hyperplasia, hypothalamic amenorrhea, and, although rare, a testosterone-secreting tumor or prolonged external exposure to androgens.
The key, Brown explains, is examining the time course of the patient’s symptoms. Whereas symptoms of PCOS are chronic and will be progressive from adolescence into adulthood, a sudden appearance or worsening of symptoms likely indicates another cause.
“Women who are diagnosed with PCOS deserve to consult with an endocrinologist or another provider with a deep knowledge of PCOS to talk about fertility, metabolic, and psychosocial issues, as well as cycle control and cosmetic concerns,” says Brown. “Having a full understanding of the condition is critical to managing their own health care and addressing prevention.”
Brown, Pereira, and their team use a mnemonic, MY PCOS (Metabolic, CYcle control, Psychosocial, Cosmetic, Ovulation and fertility, Sleep apnea), to assess and manage all facets of the syndrome. Developed by Brown and fellow Duke endocrinologist Tracy L. Setji, MD, and published in The American Journal of Medicine in October 2014, the checklist is an effective way to organize the multisystem care of women with PCOS.
“MY PCOS allows us to review each element of the condition and address the broad spectrum of issues that women with PCOS face,” says Brown. “Simply making the diagnosis can be helpful. It gives a name to the condition they’ve lived with for so long.”
“A lot of women will see their primary care provider for treatment of one of their PCOS symptoms,” explains Pereira. “It is important to ensure that all symptoms are addressed comprehensively and that metabolic risks are identified early so we can partner with the woman to implement preventive strategies.”