Welcome to Ur-BIOME!

We are dedicated to understanding microbial communities within the urogenital system to improve human health.
Our Duke Urogenital Microbiome (Ur-BIOME) Research Program includes physicians, scientists, patient advocates and trainees who are committed to driving groundbreaking research on how the urogenital microbiome shapes human health. A key focus of our work is exploring sex-specific differences in the urogenital microbiome across various life stages and understanding how these differences influence a woman’s overall well-being. Our interdisciplinary team is passionate about translating our findings into tangible benefits for others. We do this by pushing the boundaries of knowledge, training future researchers, and educating the public. Together, we embark upon a journey of discovery, innovation, and impact.
People

Silvia Grant, PhD, PMP
Research Program Leader
Originally from Switzerland, Silvia has earned her bachelor’s degree in biology and biochemistry from the University in Zurich (Switzerland) and a Ph.D. from the University of Hawai’i at Mānoa. As a laboratory research manager and senior scientist at the Institute for Genome Sciences (University of Maryland, School of Medicine), Silvia led projects focused on the gut microbiome and its clinical implications, particularly regarding the gut-brain axis. She then transitioned to a role with Metabolon, Inc., where she helped elucidate the impacts of small molecules produced by bacteria in our bodies. At Duke University, she is leading the efforts of Dr. Siddiqui and her team in understanding the effects of the urogenital microbiome on health and disease. With extensive experience in research and project management, bioinformatics, and collaborative studies, Silvia is passionate about advancing microbiome research and its impact on health. Outside of her academic interests, she loves being in nature and enjoys sharing its beauty with her husband and two daughters.
Contact information:
Email: silvia.grant@duke.edu
LinkedIn: www.linkedin.com/in/silvia-grant-phd-0977177a
Google Scholar: https://scholar.google.com/citations?hl=en&user=gVi-GtEAAAAJ

Christina Bergemann, PhD
Postdoctoral Associate
Christina received her undergraduate degree in Environmental Science from the University of North Carolina at Chapel Hill. She then worked as a technician at NC State and Duke University prior to earning her Ph.D. in the Integrated Toxicology and Environmental Health Program at Duke. Her dissertation work focused on understanding how gut microbiota could influence susceptibility to environmental chemicals. Her current research will investigate how host-microbe interactions impact recurrent urinary tract infections. In the future, she hopes to look at how environmental chemicals can impact the urogenital microbiome. Outside of the lab, she enjoys spending time outside with her husband and daughter, gardening, and biking.

Elizabeth Howell, MD
Fellow, Urogynecology and Reconstructive Pelvic Surgery
Elizabeth is originally from Atlanta, Georgia. She completed her undergraduate degree in Neuroscience at Duke University, during which time she also competed as a varsity athlete on the rowing team. Following graduation, Elizabeth accepted a gap year position as the Clinic Navigator for the Duke Brain Tumor Center. She then matriculated to Duke for medical school, where she discovered her passion for women's health, and matched at Duke for her residency in Obstetrics and Gynecology. Elizabeth has now joined the Ur-BIOME team as a fellow in Urogynecology and Reconstructive Pelvic Surgery. Elizabeth is currently investigating the impact of probiotics for patients with recurrent urinary tract infections and the role of PCR-based testing for UTIs. Outside of the hospital, Elizabeth can be found running the American Tobacco Trail, perusing the Durham farmers' market or trying a new restaurant with friends.

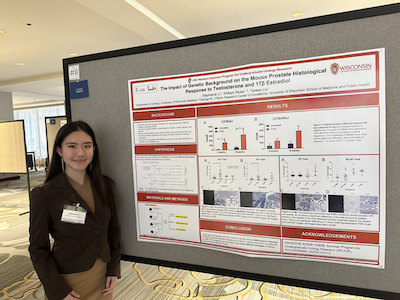
Stephanie Li, BS
Research Technician II
Stephanie is originally from San Francisco, and she earned her bachelor’s degree in Neurobiology and Criminal Justice from the University of Wisconsin-Madison. She has been involved in the Urogenital field since college when she participated in Benign Prostatic Hyperplasia research in the Wisconsin Institute of Medical Research. At Duke University, she works as a research technician at Dr. Siddiqui’s lab to further discover the role of urogenital microbiome on health. She is passionate about improving community health through innovative research. Outside of the lab, Stephanie likes to run, go to the gym, and enjoy a good coffee.

Rachel Kim
Rachel is originally from Haymarket, Virginia. She is currently a senior studying biology at Duke University and joined Ur-BIOME as an undergraduate research assistant during the summer of 2024. She started an independent study with Ur-BIOME during the spring of 2025, focusing on creating a humanized mouse model to investigate the urogenital microbiome, and is continuing this independent study into the fall semester of 2025. Rachel is interested in learning about a more preventative approach to medicine and is passionate about spreading awareness of women’s health. Outside of research, Rachel spends her time volunteering in the community as an EMT, hiking, or going to the gym.

Eve Glovinsky
Eve is originally from New Orleans, Louisiana. She is currently a junior at Duke University studying Biomedical Engineering with minors in Global Health and Chemistry. She joined Ur-BIOME in the spring of 2025 as a research assistant, working on the creation of a humanized mouse model to study the urogenital microbiome. She is passionate about advancing women’s healthcare through research and innovation. She just returned from a semester abroad in Dublin, Ireland, and in her free time, she enjoys running, climbing, and hiking.

Anna Karius
Anna is from South Carolina and is currently studying Biomedical Engineering as an undergraduate at Duke University. At Ur-BIOME, she is researching the urogenital microbiome and the feasibility of self-sampling for postmenopausal patients using vaginal estrogen. Anna's interests lie in improving women's health through research and education. She enjoys reading, being outside, and weightlifting.

Johann Galilea, BS
Born and raised in Durham, Johann earned a bachelor's degree in Biological Sciences with a concentration in Human Biology from North Carolina State University. He hopes to become a dentist and is currently applying to dentistry schools. Since graduating, Johann has joined the supply chain management team at Duke University Hospital, ordering and delivering medical supplies to patients in need throughout the hospital. Johann joined the Ur-BIOME team as a research assistant, hoping to contribute to advancements in health and microbiome research. In his free time, he loves to listen to and perform music and can play the alto saxophone, guitar, piano, and violin. He also loves basketball and proudly reps the NC State men's and women's basketball teams.
Current Research
Postmenopausal women are disproportionately affected by urinary tract infections (UTIs). Estrogen hormone therapy is an effective treatment, however, the mechanisms underlying this protection are poorly understood. The current lack of suitable animal models hinders research into how estrogen affects the human female urogenital microbiome, which in turn influences health and disease. Our research team is collaborating with Dr. Nicole De Nisco at University of Texas – Dallas to develop a germ-free mouse model that is colonized with human Lactobacillus crispatus. We hope to use this model to study the impacts of estrogen and lactobacilli on the rest of the local bladder microenvironment.
Overactive bladder (OAB), characterized by urinary urgency, frequency, and nocturia, is a complex condition with potential underlying subtypes. Previous studies have identified clinical subtypes using patient characteristics. However, a deeper understanding of the pathophysiology, particularly how the microbiome and other metabolic factors are involved, is needed. We are working with data scientists from Duke and with Dr. Lisa Karstens at Oregon Health & Science University to analyze existing data from two large cohorts. We will incorporate microbiome profiles to refine the OAB subtypes that were previously proposed (more info on NIH reporter website). By understanding OAB subtypes, we hope to better understand how to target the right treatments to the right patients.
Urinary tract infections (UTIs) are a common problem, especially for women. While sporadic UTIs are generally manageable, recurrent UTIs are more challenging due to factors like antibiotic resistance and non-standard pathogens. For females with recurrent UTI, current diagnostic methods often lack precision. The lack of precision leads to either overdiagnosis with unnecessary antibiotic prescriptions, or underdiagnosis, leading to prolonged pain and discomfort, with the potential for repeated health care visits or hospitalization. Our goal is to improve patient outcomes by improving diagnostic precision so we can quickly treat with antibiotics when needed but also avoid antibiotics when unnecessary. Our team leverages our knowledge of health care systems, clinical research, and advanced molecular testing to study how we may improve testing in women with recurrent UTIs.
For women who develop recurrent UTIs, they often swirl in patterns of repeated symptoms and repeated courses of antibiotics for months or years. There are several options for UTI prevention (including non-antibiotic prevention strategies), but these are underutilized1. Even with evidence-based ways to prevent UTIs, there are still many gaps in our knowledge of this common condition. Our team is currently working on ways to:
-
Improve public knowledge about recurrent UTIs so that women can advocate for their health and get better access to preventive care
-
Improve knowledge among health care providers to provide evidence-based non-antibiotic prevention strategies
-
Leverage the urogenital microbiome to minimize recurrent UTIs
-
Developing a workforce to keep studying these conditions in the future
While we are constantly seeking grants and funding from agencies like the National Institutes of Health (NIH), only 8.8% of the NIH budget goes to support research funding for women’s health conditions2. This includes female-specific cancers and pregnancy research, leaving only small fractions available for everything else. Therefore, we also partner with foundations and individuals to help us fund the projects listed above. If you have an area, you are passionate about, please contact us!
1Gleicher S, Sebesta EM, Kaufman MR, Dmochowski RR, Reynolds WS. Recurrent urinary tract infection management and prevention techniques among a population-based cohort of women. Neurourol Urodyn. 2023 Nov;42(8):1676-1685. doi: 10.1002/nau.25281. Epub 2023 Sep 5. PMID: 37670465.
2Burke SP, Salganicoff A, Geller A; Committee on the Assessment of NIH Research on Women's Health; Board on Population Health and Public Health Practice; Health and Medicine Division; National Academies of Sciences, Engineering, and Medicine. A New Vision for Women's Health Research: Transformative Change at the National Institutes of Health. Washington (DC): National Academies Press (US); 2024 Dec 5. PMID: 39652697.
Publications
Siddiqui, Nazema Y. MD, MHSc*; Ackerman, A. Lenore MD, PhD†; Advani, Sonali D. MBBS, MPH*; Chai, Toby MD‡; Chu, Christine MD, MSCI§; Falk, Kerac MD∥; Jeney, Sarah E.S. MD¶; Bradley, Megan MD#. Management of Asymptomatic Bacteriuria in Adult Female Populations. Urogynecology 31(9):p 827-845, September 2025. | DOI: 10.1097/SPV.0000000000001731
Luchristt, Douglas, Nazema Y. Siddiqui, Yasmeen Bruton, and Anthony G. Visco. “Response to Letter to the editor on:" Extended treatment-dose antibiotic therapy versus low-dose prophylaxis for the management of recurrent uncomplicated urinary tract infections in peri- and postmenopausal women".” Urology, February 4, 2025. https://doi.org/10.1016/j.urology.2025.01.067.
Siddiqui, Nazema Y. “Urinary Tract Infections: An Age-Old Problem that Demands New Solutions.” Obstet Gynecol 145, no. 1 (January 1, 2025): 13–14. https://doi.org/10.1097/AOG.0000000000005795.
Luchristt, Douglas, Nazema Y. Siddiqui, Yasmeen Bruton, and Anthony G. Visco. “Extended Treatment-dose Antibiotic Therapy vs Low-dose Prophylaxis for the Management of Recurrent Uncomplicated Urinary Tract Infections in Peri- and Post-menopausal Women.” Urology, December 20, 2024. https://doi.org/10.1016/j.urology.2024.12.029.
Lai, H Henry, Jerrel Rutlin, Abigail R. Smith, Margaret E. Helmuth, James A. Hokanson, Claire C. Yang, J Quentin Clemens, et al. “Structural Changes in Brain White Matter Tracts Associated With Overactive Bladder Revealed by Diffusion Tensor Magnetic Resonance Imaging: Findings From a Symptoms of Lower Urinary Tract Dysfunction Research Network Cross-Sectional Case-Control Study.” J Urol 212, no. 2 (August 2024): 351–61. https://doi.org/10.1097/JU.0000000000004022.
Advani, S. D., Claeys, K. C., & Siddiqui, N. Y. (2024). What Should I Know About Recurrent UTIs in Older Women? JAMA Intern Med, 184(8), 994. https://doi.org/10.1001/jamainternmed.2024.1854
Advani, S. D., Turner, N. A., North, R., Moehring, R. W., Vaughn, V. M., Scales, C. D., … Anderson, D. J. (2024). Proposing the "Continuum of UTI" for a Nuanced Approach to Diagnosis and Management of Urinary Tract Infections. J Urol, 211(5), 690–698. https://doi.org/10.1097/JU.0000000000003874
Jiang, D., Soo, N., Tan, C. Y., Dankwa, S., Wang, H.-Y., Theriot, B. S., … Surana, N. K. (2024). Commensal bacteria inhibit viral infections via a tryptophan metabolite. BioRxiv. https://doi.org/10.1101/2024.04.21.589969
London, L. Y., Lim, C. H., Modliszewski, J. L., Siddiqui, N. Y., & Sysoeva, T. A. (2023). Draft genomes of Lactobacillus delbrueckii and Klebsiella pneumoniae coexisting within a female urinary bladder. Microbiol Resour Announc, 12(10), e0030523. https://doi.org/10.1128/MRA.00305-23
Vaughan, M. H., Zemtsov, G. E., Dahl, E. M., Karstens, L., Ma, L., & Siddiqui, N. Y. (2022). Concordance of urinary microbiota detected by 16S ribosomal RNA amplicon sequencing vs expanded quantitative urine culture. Am J Obstet Gynecol, 227(5), 773–775. https://doi.org/10.1016/j.ajog.2022.06.031
Johnson, J. A., Modliszewski, J. L., Siddiqui, N. Y., & Sysoeva, T. A. (2022). Draft Genome Sequence of a Lactobacillus gasseri Strain Isolated from the Catheterized Urine of a Healthy Postmenopausal Woman. Microbiol Resour Announc, 11(6), e0002122. https://doi.org/10.1128/mra.00021-22
Hendrickson, W. K., Havrilesky, L., & Siddiqui, N. Y. (2022). Cost-effectiveness of bacteriuria screening before urogynecologic surgery. Am J Obstet Gynecol, 226(6), 831.e1-831.e12. https://doi.org/10.1016/j.ajog.2021.11.1375
Richter, H. E., Carnes, M. U., Komesu, Y. M., Lukacz, E. S., Arya, L., Bradley, M., … Eunice Kennedy Shriver National Institute of Child Health and Human Development Pelvic Floor Disorders Network. (2022). Association between the urogenital microbiome and surgical treatment response in women undergoing midurethral sling operation for mixed urinary incontinence. Am J Obstet Gynecol, 226(1), 93.e1-93.e15. https://doi.org/10.1016/j.ajog.2021.07.008
Johnson, J. A., Delaney, L. F., Ojha, V., Rudraraju, M., Hintze, K. R., Siddiqui, N. Y., & Sysoeva, T. A. (2022). Commensal Urinary Lactobacilli Inhibit Major Uropathogens In Vitro With Heterogeneity at Species and Strain Level. Front Cell Infect Microbiol, 12, 870603. https://doi.org/10.3389/fcimb.2022.870603
Siddiqui, N. Y., Ma, L., Brubaker, L., Mao, J., Hoffman, C., Dahl, E. M., … Karstens, L. (2022). Updating Urinary Microbiome Analyses to Enhance Biologic Interpretation. Front Cell Infect Microbiol, 12, 789439. https://doi.org/10.3389/fcimb.2022.789439
Zemtsov, G. E., Vaughan, M. H., Dahl, E. M., Karstens, L., Ma, L., & Siddiqui, N. Y. (2022). Concordance of Urinary Microbiota Detected by 16S rRNA Amplicon Sequencing Versus Expanded Quantitative Urine Culture. In INTERNATIONAL UROGYNECOLOGY JOURNAL (Vol. 33, pp. S219–S220).
Vaughan, M. H., Mao, J., Karstens, L. A., Ma, L., Amundsen, C. L., Schmader, K. E., & Siddiqui, N. Y. (2021). The Urinary Microbiome in Postmenopausal Women with Recurrent Urinary Tract Infections. The Journal of Urology, 206(5), 1222–1231. https://doi.org/10.1097/ju.0000000000001940
Siddiqui, N. Y. (2021). Editorial Comment. J Urol, 206(5), 1221. https://doi.org/10.1097/JU.0000000000001949.02
Hoffman, C., Siddiqui, N. Y., Fields, I., Gregory, W. T., Simon, H. M., Mooney, M. A., … Karstens, L. (2021). Species-Level Resolution of Female Bladder Microbiota from 16S rRNA Amplicon Sequencing. MSystems, 6(5), e0051821. https://doi.org/10.1128/mSystems.00518-21
Brubaker, L., Gourdine, J.-P., Siddiqui, N. Y., Holland, A., Halverson, T., Limeria, R., … Wolfe, A. J. (2021). Forming Consensus To Advance Urobiome Research. MSystems, 6(4), e0137120. https://doi.org/10.1128/msystems.01371-20
Bickhaus, J. A., Bradley, M. S., Amundsen, C. L., Visco, A. G., Truong, T., Li, Y. J., & Siddiqui, N. Y. (2021). Does a recent urinary tract infection increase the risk of postprocedure urinary tract infection after onabotulinum toxin a? Obstetrical and Gynecological Survey, 76(5), 267–268. https://doi.org/10.1097/01.ogx.0000751432.28331.65
Karstens, L., Siddiqui, N. Y., Zaza, T., Barstad, A., Amundsen, C. L., & Sysoeva, T. A. (2021). Benchmarking DNA isolation kits used in analyses of the urinary microbiome. Sci Rep, 11(1), 6186. https://doi.org/10.1038/s41598-021-85482-1
Bickhaus, J. A., Bradley, M. S., Amundsen, C. L., Visco, A. G., Truong, T., Li, Y.-J., & Siddiqui, N. Y. (2021). Does a Recent Urinary Tract Infection Increase the Risk of Postprocedure Urinary Tract Infection After Onabotulinum Toxin A? Female Pelvic Med Reconstr Surg, 27(2), 121–125. https://doi.org/10.1097/SPV.0000000000000753
Vaughan, M. H., Mao, J., Karstens, L. A., Ma, L., Amundsen, C. L., Schmader, K. E., & Siddiqui, N. Y. (2021). The Urinary Microbiome in Postmenopausal Women with Recurrent Urinary Tract Infections. JOURNAL OF UROLOGY, 206(5), 1223–1231.
Bickhaus, J. A., Vaughan, M., Truong, T., Li, Y.-J., & Siddiqui, N. Y. (2020). A comparison of antibiotic prophylaxis regimens to decrease the risk of post-procedure urinary tract infection after onabotulinum toxin A injection. Int Urogynecol J, 31(9), 1907–1912. https://doi.org/10.1007/s00192-020-04230-7
Siddiqui, N. Y., Vaughan, M. H., Ma, L., Karstens, L., Amundsen, C., & Schmader, K. (2020). Urinary Microbiome in Menopausal Women with Recurrent Urinary Tract Infections. In JOURNAL OF THE AMERICAN GERIATRICS SOCIETY (Vol. 68, pp. S11–S11). Long Beach, CA: WILEY.
Komesu, Y. M., Dinwiddie, D. L., Richter, H. E., Lukacz, E. S., Sung, V. W., Siddiqui, N. Y., … Eunice Kennedy Shriver National Institute of Child Health and Human Development Pelvic Floor Disorders Network. (2020). Defining the relationship between vaginal and urinary microbiomes. Am J Obstet Gynecol, 222(2), 154.e1-154.e10. https://doi.org/10.1016/j.ajog.2019.08.011
Siddiqui, N. Y., Helfand, B. T., Andreev, V. P., Kowalski, J. T., Bradley, M. S., Lai, H. H., … Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN). (2019). Biomarkers Implicated in Lower Urinary Tract Symptoms: Systematic Review and Pathway Analyses. J Urol, 202(5), 880–889. https://doi.org/10.1097/JU.0000000000000257
Komesu, Y. M., Richter, H. E., Carper, B., Dinwiddie, D. L., Lukacz, E. S., Siddiqui, N. Y., … Pelvic Floor Disorders Network. (2018). The urinary microbiome in women with mixed urinary incontinence compared to similarly aged controls. Int Urogynecol J, 29(12), 1785–1795. https://doi.org/10.1007/s00192-018-3683-6
Arya, L. A., Richter, H. E., Jelovsek, E., Gantz, M., Cichowski, S., Zyczynski, H., … Meikle, S. (2018). Metabolites and microbial composition of stool of women with fecal incontinence: Study design and methods. Neurourol Urodyn, 37(2), 634–641. https://doi.org/10.1002/nau.23360
Polin, M. R., Kawasaki, A., Amundsen, C. L., Weidner, A. C., & Siddiqui, N. Y. (2017). Do Mixed-Flora Preoperative Urine Cultures Matter? South Med J, 110(6), 426–429. https://doi.org/10.14423/SMJ.0000000000000659
Komesu, Y. M., Richter, H. E., Dinwiddie, D. L., Siddiqui, N. Y., Sung, V. W., Lukacz, E. S., … Gantz, M. (2017). Methodology for a vaginal and urinary microbiome study in women with mixed urinary incontinence. Int Urogynecol J, 28(5), 711–720. https://doi.org/10.1007/s00192-016-3165-7
Events
Ur-BIOME team members regularly attend conferences such as ASM, AUGS, and CAIRIBU, with plans to participate in additional meetings in the future. We strive to present more of our research to the urogenital microbiome community and connect with other researchers/collaborators. We always look forward to connecting with fellow researchers and are excited to set up meetings at any of the conferences we will attend, which are listed below with more to come.
Future Events
ASM Microbe 2026
June 4-7, 2026
The Ur-BIOME team will attend ASM Microbe 2026, taking place June 4–7 in Washington, DC. ASM Microbe 2026 brings together three co-located meetings spanning clinical and public-health microbiology, applied and environmental microbiology, and fundamental mechanism discovery. We are pleased to share that our proposed session, “Translating Urogenital Microbiome Science into Clinical Impact,” has been accepted, providing a dedicated forum to highlight advances in urogenital microbiome research to a broad scientific audience. Dr. Nazema Siddiqui, MD, MHSc, will serve as the invited speaker, with moderation by Dr. Diane Alame, MD, MBE, a clinical pathologist and medical microbiologist at Duke University.
Past Events
CAIRIBU 2025

December 3-5, 2025


AUGS PFD Week 2025

October 14-17, 2025
ASM Microbe 2025

June 19-23, 2025
ASM Microbe is the largest microbial sciences gathering in the world. Experts around the world including John Helmann, PhD, and Anne W. Rimoin, PHD, are lined up in ASM Microbe’s cutting-edge scientific program. These experts curated groundbreaking scientific sessions on topics that are shaping the future of humanity. It includes various fields within microbiology, from microbial solutions to global problems to artificial intelligence research.


UROBIOME 2025

February 24th, 2025
Urobiome is a groundbreaking in-person event exploring the latest advancements in understanding the urobiome. Experts in the field will share their research and insights on how the urobiome influences our health, including common conditions such as UTI, urinary incontinence, and bladder overactivity. This day-long conference is located at Scripps Institution of Oceanography. It is filled with insightful talks, interactive roundtables, and various networking opportunities.

CAIRIBU 2024

December 4-6, 2024
CAIRIBU is a community of NIDDK-funded benign urology research centers and programs. The purpose of the annual meeting is to bring together the directors and research teams and share various research resources. This meeting aims to advance students and early investigators in their development as future leaders in the field of benign urology. This two-and-a-half-day meeting entails poster sessions featuring the works of trainees and early-stage investigators, and scientific sessions featuring esteemed researchers in the field.
AUGS PFD Week 2024

October 22-25, 2024
AUGS PFD Week brings together health care professionals in the field of Urogynecology and Reconstructive Pelvic Surgery to collaborate, network, and learn from other’s expertise. PFD Week creates a forum to exchange knowledge, experience, and insights for the improvement of women’s urogynecologic care. The core of the meeting contains two and a half days of scientific presentation with the addition of one day of surgical and clinical workshop sessions.
Get Involved
For those interested in being involved in our research, please get in touch with Silvia Grant, Ur-BIOME Research Program Leader, by email at silvia.grant@duke.edu.
We have various types of student engagements, most notably our monthly “journal club” style meetings during which we discuss the latest research articles on the urogenital microbiome. We always welcome more diverse opinions from individuals to contribute to our discussion.

If you want to dedicate more time in our lab, we are supporting undergraduate students who want to conduct their independent study in our research group. Feel free to email us and find out more about current opportunities.
We are also open to graduate students, residents, and fellows who want to collaborate with us on their thesis projects.
Become an Advocate
We invite former and current patients to join us as advocates in our research journey. Your unique experiences and insights are invaluable in shaping studies that truly address patient needs and priorities. By becoming an advocate, you will have the opportunity to actively contribute to decision-making, bridge the gap between research and real-world impact, and ensure that patient voices are heard. Together, we can create research that makes a difference - your voice matters, and we would love to have you involved!
For more information about how to become an advocate, please contact Silvia Grant, Ur-BIOME Research Program Leader, by email at silvia.grant@duke.edu.
Looking for a way to help?
Contribute to the Duke Urogenital Microbiome Research Program (Ur-BIOME).
There are many ways to make a gift to the Duke Urogynecology Research Program (Ur-BIOME). For more information about giving, please contact Jillian Ream, Senior Executive Director of Development, Duke Health Development and Alumni Affairs, by calling 919-385-3197 or by email at jillian.ream@duke.edu.


