2026 Symposium featuring:
Urogenital Pain | Obesity Effects on Urogenital Conditions

Friday
April 17, 2026

8 a.m.- 4 p.m.

Trent Semans Center
Great Hall
Panel Discussions * Trainee Platform Presentations * Poster Sessions * Lunch with Experts * Trainee Abstract Awards * Trainee Travel Awards
Faculty, fellows, postdocs, students and staff from any discipline are encouraged to attend.
| TIME | SESSION |
|---|---|
| 8:00 AM | Check in |
| 8:15 AM | Welcome & Introductions |
| 8:25 AM | Trainee Podium Presentations |
| 9:30 AM | Poster Session 1 |
| 10:35 AM |
Panel: Urogenital Pain
Discussion |
| 11:40 AM | Lunch or Conversations and Lunch with the Experts |
| 12:45 PM | Poster Session 2 |
| 1:50 PM |
Panel: Obesity Effects on Urogenital Conditions
Discussion |
| 3:00 PM | Trainee Podium Presentations |
| 3:50 PM | Evaluations |
| 3:55 PM |
Presentation of Trainee Awards and Closing Remarks |
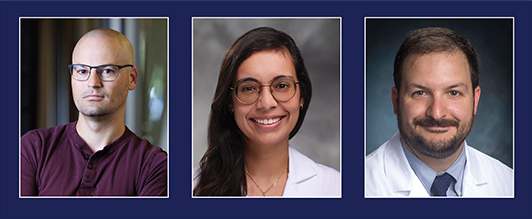
Panel: Urogenital Pain
Dr. Clemens is internationally recognized for his expertise in functional urology. He obtained his MD degree from the Johns Hopkins University School of Medicine. He completed his urologic residency training at Northwestern University Medical School and his Fellowship in Neurourology, Reconstruction and Incontinence at the University of Michigan. Dr. Clemens is the Edward J. McGuire Professor of Urology, Associate Chair for Research, and Director of the Urogynecology and Reconstructive Pelvic Surgery Fellowship Program. Dr. Clemens’ research interests are in the areas of epidemiology and health services research related to benign urologic diseases. He has published over 300 peer-reviewed manuscripts and book chapters and has had continuous NIH funding since 2001. He has been Principal Investigator on multiple NIH-funded projects related to urinary incontinence, interstitial cystitis and chronic prostatitis, including the NIDDK MAPP Research Network and NIDDK LURN Research Network.
Dr. Nackley is an Associate Professor of Anesthesiology and Associate Director of the Center for Translational Pain Medicine at Duke University. She is Director of the Translational Pain Research Laboratory, where her program marries pain neurobiology, behavioral pharmacology, and molecular genetics in mouse and man to better understand what causes chronic pain and how to effectively treat it. During the past 20 years, her expertise in this area has been applied to the study of how alterations in gene regulation, protein expression, and receptor signaling contribute to chronic ‘primary’ overlapping pain conditions such as vestibulodynia. Her lab was the first to demonstrate a critical role for peripheral adrenergic receptor beta-3 in the development of chronic pain and neuroinflammation, which remains a primary research focus. Dr. Nackley is an active leader in the field, participating in pain-relevant workshops and delivering invited lectures around the globe. In recognition of her scholarly activity in the Pain field, she received the John C. Liebeskind Career Scholar Award from the American Pain Society.
Dr. Walker is a geneticist and molecular biologist with a focus on systems biology and diagnostic biomarker discovery in complex disorders. Since 2014, one primary focus of his research has been to leverage molecular, histological, and cellular data, together with clinical and demographic information, for the identification of clinically relevant patient subgroups in interstitial cystitis/bladder pain syndrome. The overall goal is to identify mechanisms underlying specific subgroup pathophysiology so that regenerative medicine and other therapeutic strategies can be used to improve treatment outcomes for this highly heterogeneous patient population. A secondary goal is to partner with other experts in the field (e.g., clinicians and basic scientists new to benign urology research) to enhance our capabilities and accelerate our progress towards the overall goal.
Panel: Obesity Effects on Urogenital Conditions
Dr. Campbell is an Associate Professor at Duke University in the Department of Medicine and the Department of Pharmacology and Cancer Biology, as well as a faculty member of the Duke Molecular Physiology Institute (DMPI). His background is in biology and physiology, with specific training and expertise in diabetes, islet biology, and gut hormone endocrinology. His research program, located in the Duke Molecular Physiology Institute, uses preclinical models including cell-based assays, genetic mouse models, and human samples to investigate the various mechanisms of action for incretins in physiology and pharmacology. His group also translates the results from preclinical models through human physiology studies. The current focus of his group is to: 1) understand the unique and common signaling pathways engaged by incretins that regulate cellular function, 2) elucidate the importance of paracrine interaction within the islet, and 3) determine novel mechanisms by which incretin peptides and glucagon interact to regulate metabolism.
Dr. Sinha is a board-certified obstetrician-gynecologist and Clinical Associate at Duke University, where she is completing a fellowship in Urogynecology and Female Pelvic Reconstructive Surgery. She earned her MD from Case Western Reserve University and completed residency at the Cleveland Clinic Foundation. Her research focuses on pelvic floor disorders, voiding dysfunction, and Bayesian adaptive trial design. Dr. Sinha has authored numerous peer-reviewed publications and presented nationally on topics including nocturia, cardiovascular risk, and surgical optimization. After graduation, she plans to join the Division of Urogynecology and Reconstructive Pelvic Surgery at the Medical College of Georgia at Augusta University as an academic urogynecologist.
Dr. Wood joined the University of Alabama at Birmingham, Department of Urology in July 2016. He attended medical school at University of Massachusetts, and completed his residency at Wake Forest University. Dr. Wood is fellowship trained in Endourology with a primary focus on kidney stone disease. His surgical expertise is in complex kidney stone disease and surgeries. He is a trained open, endoscopic, laparoscopic and robotic surgeon. The focus of multidisciplinary metabolic kidney stone clinic is on the workup of kidney stone formers and implementing dietary, medical and lifestyle modifications to prevent future kidney stones. He is an AUA research scholar and is conducting kidney stone research on the metabolic pathways that lead to kidney stone disease, specifically evaluating the role of obesity in kidney stone disease. His research has basic, translational and clinical components.
Past Symposia
10th Annual Multidisciplinary Benign Urology Research Symposium (2025)
April 9, 2025 - Duke University
Program Booklet Recording Photo Gallery
Podium Presentation Awardees
Top Basic Science Abstracts
Ananya Pinnamaneni - Duke University
- Estrogen-dependent mechanisms increase urothelial c-fiber populations and contribute to the pathogenesis of overactive bladder in female type 1 diabetic Akita mice
Gabriella Robilotto, BS - Medical College of Wisconsin
- Optical inhibition of OPN3 with transdermal light reduces nociceptive behaviors in mice with acute cystitis
Top Translational Science Abstract
Mina Ghatas, MS - Virginia Commonwealth University
- A preliminary study utilizing Bladder NIRS as a non-invasive approach to detect detrusor overactivity in patients with OAB
Top Clinical Science Abstracts
Bin Ni, MD, PhD - Duke University
- Assessing incidence, risk factors, and outcomes of BK virus- related complications following kidney transplantation
Aaron Stewart, MD – Duke University
- Enhancing urology referral intake through artificial intelligence-assisted pre-charting: a pilot study
Poster Presentation Awardees
Basic Science
Samantha McGuire, MS - Eastern Virginia Medical School
- Cxcl17 Alters urinary function but does not affect foam cell formation in the mouse prostate
Translational Science
Priyanka Saraf, BA - Virginia Commonwealth University
- Association between bladder shape and detrusor overactivity in ultrasound urodynamics
Clinical Science
Jasmine Arrington, MD, MPH - Duke University
- Nocturia and falls associations among Lower Urinary Tract Network cohort



Friday, April 19, 2024 - 8:00AM - 4:30PM - Duke University - Trent Semans Great Hall
Panel Discussions * Trainee Platform Presentations * Poster Sessions * Lunch with Experts * Trainee Abstract Awards * Trainee Travel Awards
Platform Presentation Awardees
Top Basic Science Abstract
Samara Silver, BS, Eastern Virginia Medical School
Characterization of foam cells and lipid dysregulation in benign prostate disease in men and mouse models
Top Translational Science Abstract
Cassandra Kisby, MD, Duke University School of Medicine
Exosome injection as a prevention strategy for mesh complications in a porcine model of sacrocolpopexy
Top Clinical Science Abstract
Rory Ritts, MD, Wake Forest University School of Medicine
High autonomic symptom load in IC/BPS Patients correlates with a non-bladder-centric phenotype
Poster Presentation Awardees
Basic Science
Kaylie Hintze, BS (mentee of alumni scholar, Tanya Sysoeva)
University of Alabama Huntsville
Analysis of competition amongst Lactobacilli isolated from the human urinary tract
Translational Science
Diana Aponte, MD (mentee of alumni scholar, Jonathan Routh)
Duke University
Assessing financial toxicity in pediatric urology: validation of a patient-reported outcome measure tool in spina bifida
Clinical Science
Mary Namugosa, MD
Wake Forest School of Medicine
Frailty is common in older interstitial cystitis/bladder pain syndrome patients with a non-bladder-centric phenotype
April 20, 2023 Duke Trent Semans Center
* Panel Discussions * Trainee Platform Presentations * Poster Sessions * Lunch with Experts * Trainee Abstract Awards * Trainee Travel Awards
Program Booklet Video Recording
A successful and exciting gathering! The 8th Annual Multidisciplinary K12 Benign Urology Research (KURe) Symposium attracted over 80 attendees from a wide range of scientific backgrounds representing 16 U.S. and Canadian academic institutions.
Congratulations to the 2023 Award Winners
Platform Presentation Awardees
Top Basic Science Abstract: Byron Hayes, PhD, Duke University
Nerve growth factor drives sensory nerve sprouting and persistent pain after recurrent bladder infection
Top Basic Science Abstract: Michael Odom, PhD, Duke University
Underactive bladders from type 1 diabetic Akita female mice exhibit an increase in contractility via FP receptor activation as a result of NLRP3-mediated inflammation
Top Translational Science Abstract: Nicole Diaz, Duke University
Aging and the female urinary microbiome: associations between Lactobacilli, menopause, and vaginal estrogen use
Top Clinical Science Abstract: Robert Medairos, MD, Duke University
The impact of single use cystoscopes on clinical time workflow in an outpatient setting
Poster Presentation Awardees
Basic Science
Aya Hajj, MSc, McGill University
Improvement in bladder parameters of 12-month-old male and female mice with THX-B treatment, an antagonist to the P75NTR receptor
Translational Science
Bradley Barth, PhD, Duke University
Sacral nerve stimulation for constipation in virtual and rodent colons
Clinical Science
Gregory Vurture, MD, Jersey Shore University Medical Center
Barriers to adherence to overactive bladder treatment for Hispanic women
Sponsors
NIH-NIDDK K12DK100024 (KURe); Duke Departments of Obstetrics & Gynecology, Urology and Biomedical Engineering; CAIRIBU